You are here
Choosing a vaccination strategy to deal with Covid variants
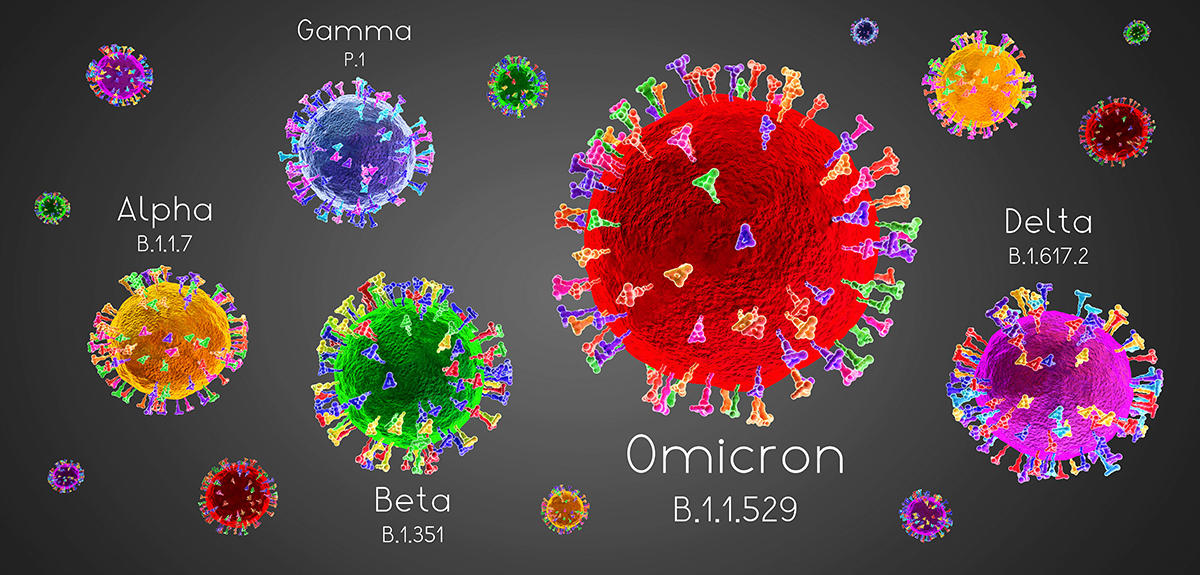
On 27 December 2020, France launched its vaccination campaign against Covid, hoping for a rapid end to the pandemic. A week previously, the alpha variant – the first in a list that would lead to Omicron – had been detected for the first time outside the United Kingdom. Although vaccines proved their ability to reduce the risks of developing severe forms of the disease, it was found as new variants emerged that they were much less effective in protecting against contamination. Vaccination strategies therefore had to evolve in order to try and respond to a never-ending health crisis. Sylvain Gandon, a CNRS research professor at the Ecology and Evolutionary Ecology research centre (CEFE)1 and his colleague Sébastien Lion have just published an article in the prestigious journal PNAS2 regarding the links between the different approaches to vaccination and how it can be adapted to the Covid virus.3
Who should be vaccinated?
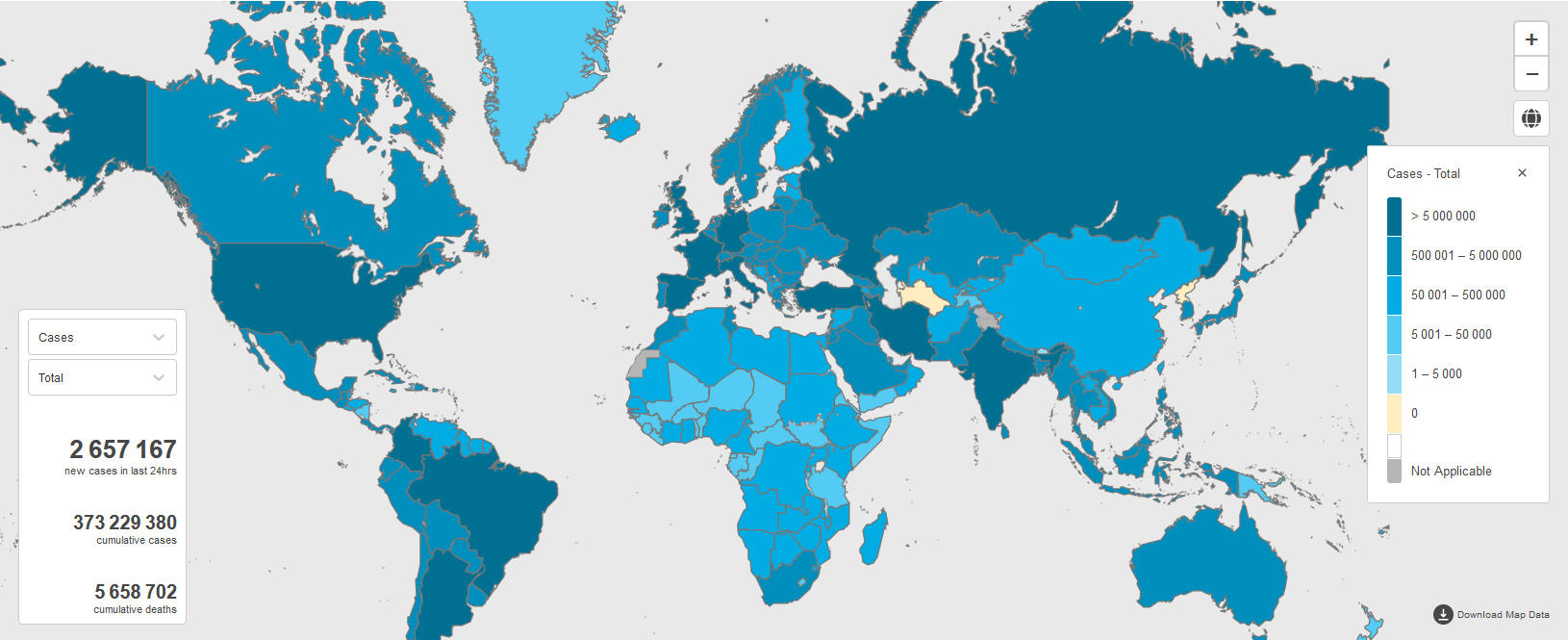
“Our work was carried out at the national scale,” explains Gandon. “Vaccination coverage varies considerably between countries; some have high inoculation rates, which on the other hand are very low in other parts of the world. The virus is therefore circulating more in certain populations, causing both ethical problems and the emergence of new variants. Our publications have not touched on access to vaccination in certain countries, but this issue certainly needs to be addressed.”

In fact, national divergences in vaccination strategies have been emphasised by the regular appearance of new variants that make decision-making difficult because of changes to their contagiousness and resistance to vaccines. All the more so in a context where insufficient doses or personnel are available to rapidly implement a full inoculation schedule for an entire population.
“Knowing who to vaccinate as a priority predates the Covid pandemic,” Gandon points out. “Should we focus on elderly and frail individuals with a greater risk of dying, or on the contrary on those who are less susceptible but more likely to spread the disease, such as young people? We need to weigh up the direct and indirect benefits of vaccination in order to minimise the number of deaths. It is a difficult problem, the solution to which changes as a function of an epidemic and its context. In the case of influenza, for example, France has chosen to immunise the elderly, while in the US, the focus is on children because the virus circulates widely in schools.”
Combining epidemiology and evolutionary biology
In the current context, standard schedules need in any case to be reviewed on a regular basis, if possible with assistance from scientists. “I would first of all like to clarify some confusing arguments reported by the media or published in the scientific literature,” Gandon insists. “It is necessary to make a distinction between how quickly variants adapt and the risk that a new one may emerge. The assertion that progress in vaccination accelerates adaptation of the virus only concerns variants that are already present. Vaccination does indeed limit the emergence of new variants because the less the pathogen is circulating, the fewer opportunities it has to mutate. With my co-author, we are firmly convinced that immunisation is a weapon to fight adaptation of the virus and protect ourselves from Covid.”
Current research work is based on both epidemiology and evolutionary biology, considering that mutations of the virus influence the dynamics of the pandemic which, in return, may favour the appearance of new variants if the disease circulates at high levels. With their Canadian colleagues, Gandon and Lion produced an initial update4 on the evolutionary potential of SARS-CoV-2 before the alpha variant even appeared. Because no vaccine was yet available at that time, they studied the impact of non-pharmaceutical control strategies (such as social distancing and protective measures) on the speed of variant spread.
“We found it difficult to publish this work because at that time many experts doubted that the virus was able to adapt so well,” Gandon recalls. “What we anticipated was ultimately observed, and particularly the selection of more transmissible variants.” These predictions were based on similar models to those used in the PNAS study to evaluate vaccination strategies.
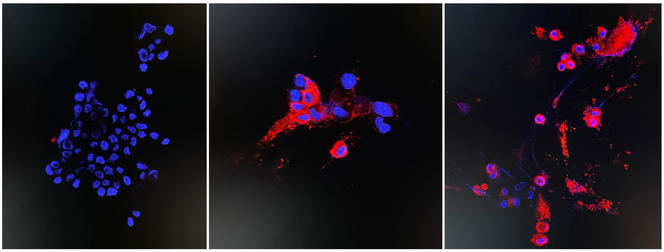
Quantifying the benefits of different strategies
In this article, the two scientists have proposed a theoretical framework that could formalise the effects – notably on variants – of various approaches to targeted vaccination. It has highlighted a constant state of tension between the speed of adaptation of the virus – i.e. the rate at which the frequency of a vaccine-resistant variant increases – and a reduction in the number of deaths, the latter parameter remaining the primary objective. Two scenarios were thus studied.
The first one compared vaccination targeting primarily the elderly, who are more fragile but contribute less to the dissemination of the virus, and an approach focusing on young people who spread the disease more easily because they have more contacts. It was found that the first option limited both the speed of adaptation and the total number of deaths. By immunising the elderly, it was possible to enjoy both the direct benefit of vaccination, which protects the most vulnerable, and the indirect benefit, which reduces selection pressure on adaptation to vaccines. This was in line with the policy adopted in France.
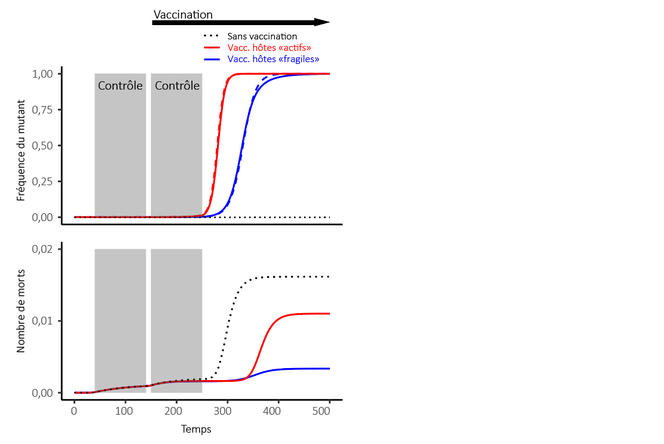

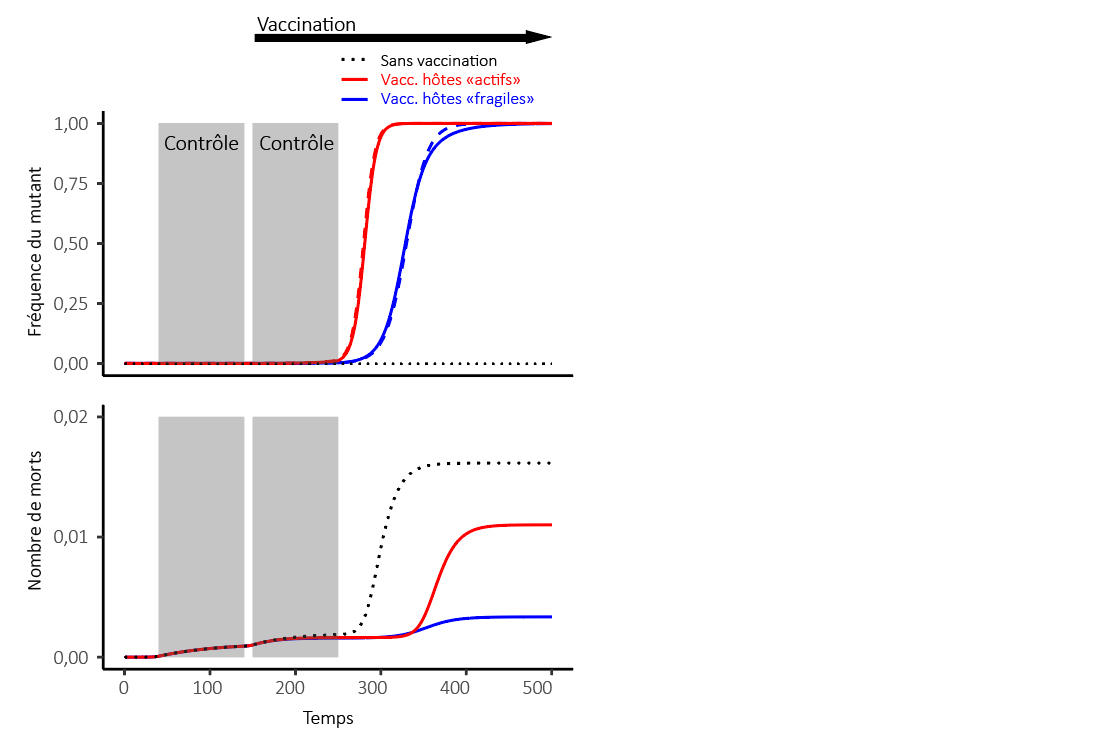
Under a second scenario, the scientists studied the effects of a strategy designed to delay the second dose so as to rapidly confer partial immunity on the greatest number of individuals, as opposed to the standard vaccination schedule with two injections at close intervals. Giving one dose to as many people as possible would accelerate adaptation of the virus, but the models indicated that a global reduction in contaminations actually helped curb the number of deaths. This showed that slowing the speed of adaptation does not necessarily limit the number of fatalities.
“We are trying to contribute our findings, but the context of vaccination is not an easy one,” concludes Gandon. “It is necessary to quantify as many acceptable arguments as possible and take objective criticisms regarding the costs of vaccination into consideration, before integrating all the data in our models.” For example, the researcher points to the existence of other epidemiological approaches which, instead of the number of deaths, take account of the years of life lost. Put simply, the deaths of individuals who are elderly or already sick do not carry the same weight in this case as those of young people previously in good health.
This is a dilemma that goes back to the early days of modern vaccination. Thus in the 18th century, the physician, physicist and mathematician Daniel Bernoulli formalised the usefulness of smallpox inoculation in a context where this method was much more dangerous than today’s vaccines. The Swiss polymath concluded that variolisation could provide an average gain of three years in life expectancy. This prediction was immediately criticised by another savant of the period, the French encyclopaedist Jean Le Rond d’Alembert, who among other things reproached his Swiss counterpart for attributing the same value to the lives of children and the elderly. This goes to show that these ethical questions are as old as the first vaccination models.

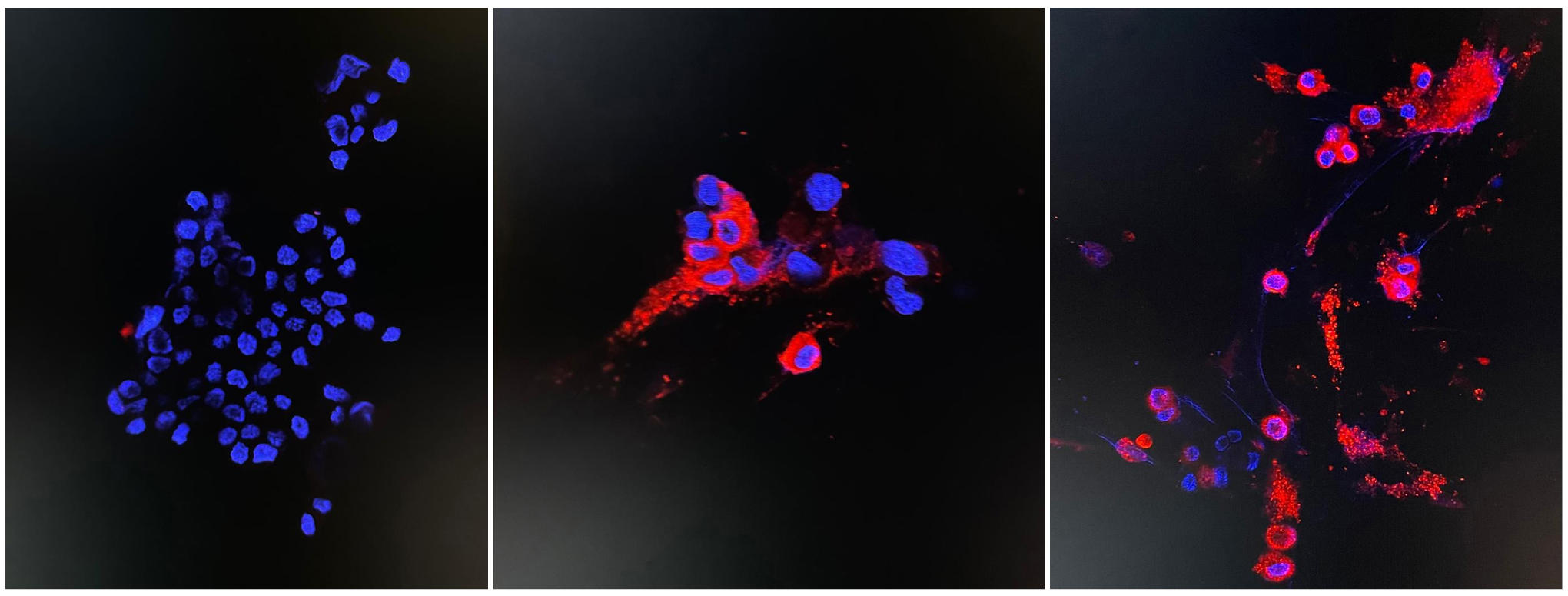
Mutations, variants and immunisation
The results obtained by Gandon and his colleagues highlight two separate phases in a pandemic.To begin with, the virus has access to a multitude of unprotected hosts. People will initially develop immunity either by getting infected or through vaccination. The pathogen will then adapt in order to try and escape this immunity, at least partly. This is what has happened with the Omicron variant, whose reduced virulence should nevertheless not raise false hopes regarding an end to the pandemic in the near future.
“With the rapid spread of Omicron, a type of herd immunity will appear,” Gandon admits. “But this will only last for a while and fragile individuals will once again be at the mercy of future waves and mutations. And although Omicron seems to be less virulent, it is sufficiently dangerous to cause much more damage among the most vulnerable in the meantime. To limit the number of deaths, it will certainly be necessary to devise new and better adapted vaccines, and monitor the evolution of the pandemic, step by step.”
In an article currently under revision, the scientist is indeed looking beyond the notion of variants to focus – at a more precise and complex level – on the mutations that give rise to them. Indeed, some of these mutations are shared by several variants, which could recombine to form new types of virus. Vaccination strategies so far have taken insufficient account of this possibility.
- 1. CNRS /EPHE / IRD / Université de Montpellier.
- 2. Proceedings of the National Academy of Sciences.
- 3. Sylvain Gandon, Sébastien Lion. “Targeted vaccination and the speed of SARS-CoV-2 adaptation”. Proceedings of the National Academy of Sciences Jan 2022, 119. DOI: 10.1073/pnas.2110666119
- 4. Day, T., Gandon, S., Lion, S., & Otto, S. P. “On the evolutionary epidemiology of SARS-CoV-2”. Current Biology, 30(15), R849-R857. 2020.
Explore more
Author
A graduate from the School of Journalism in Lille, Martin Koppe has worked for a number of publications including Dossiers d’archéologie, Science et Vie Junior and La Recherche, as well the website Maxisciences.com. He also holds degrees in art history, archaeometry, and epistemology.