You are here
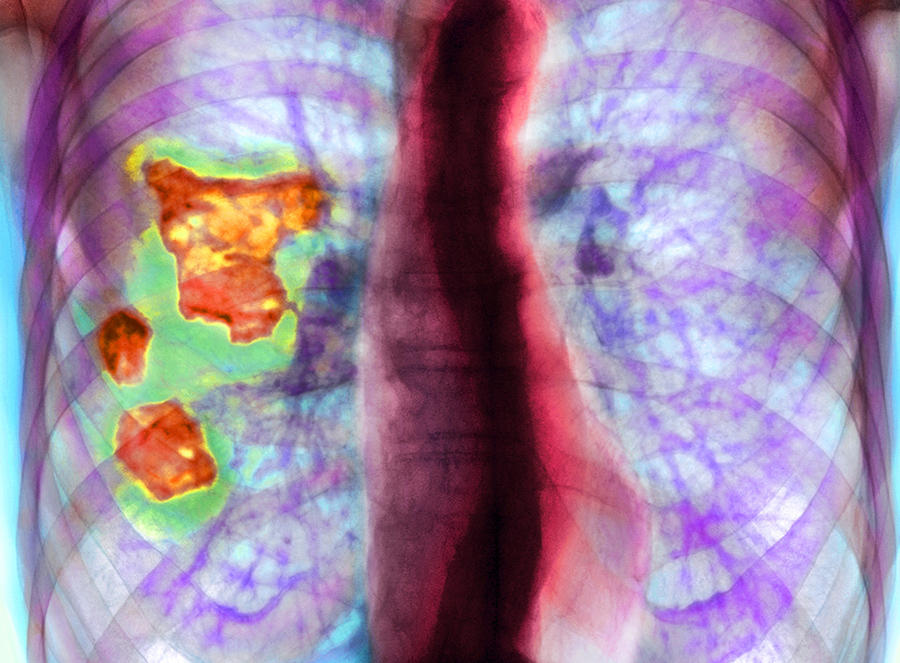
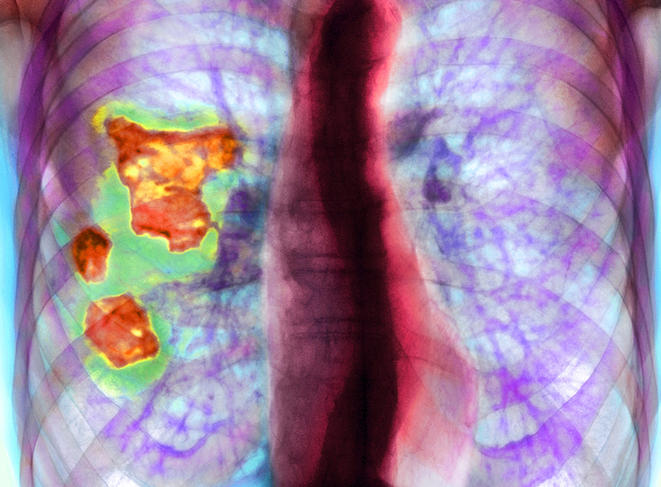
The exposome, exposure of a lifetime

Atmospheric pollutants, smoking, endocrine disruptors, radiation, diet or social inequalities…. 70% of non-transmissible diseases in humans may originate from the environment. After decades of exploring the genetic origins of human pathologies, the concept of the exposome is now seen as a complement to the “all-genetic” theory when trying to identify environmental factors. The aim is to trace all exposures in a human being – from embryo to death – and elucidate how these different substances interact during a lifetime, while taking into account behaviours, the socioeconomic environment and psychological status. And without losing sight of the fact that one type of exposure can provide the foundations for another, which may appear in later years. In 2005, Dr Christopher Wild, now director of the International Agency for Research on Cancer, laid the groundwork for the exposome concept. In an article published in Cancer Epidemiology, Biomarkers & Prevention,1 the epidemiologist defined the exposome as “the exposures that occur during a lifetime, from the prenatal period onwards. It is a complex and dynamic representation that integrates the chemical, microbiological, physical, recreational and medicinal environments, lifestyle, diet and infections”. At the time, Wild described this as an “exceptional challenge” for science.
The role of the social environment
Fifteen years on, the definition of the exposome has evolved in order to federate a variety of research fields, ranging from toxicology to epidemiology, ecology and the social sciences. Indeed, in 2012, Wild refined his concept to propose a trio of exposomes: the internal exposome (hormones, inflammatory stress markers or metabolites), the specific external exposome (pollutants, radiation, infectious agents, professional occupation and lifestyle) and the general external exposome, which concerns the socioeconomic setting and living conditions.
“Today, much more emphasis is being placed on social factors as major determinants of health: difficult social conditions mean being more likely to live near a busy road, in a noisy environment, probably eating foods of poorer quality and being subjected to higher levels of stress,” explains Dr Robert Barouki, toxicologist and director of the Inserm Environmental Toxicity, Therapeutic Targets,
Cellular Signaling and Biomarkers laboratory (T3S) at Université Paris Cité.
Highlighting the links between health and the environment does not date back to 2005. Two and a half thousand years ago, in an attempt to improve care, Hippocrates asked that “consideration be given first of all to the seasons of the year, the quality of water and winds, the different types of soil and the living conditions of inhabitants”. Then, before the First World War, “health focused more on managing the environment through hygiene, dealing with waste or water, the latter having been identified by John Snow as a vector for cholera in the mid-19th century”, points out Valérie Siroux, an epidemiologist and joint leader of the Environmental Epidemiology applied to Development and Respiratory Health (EDES) team at the Institute for Avanced Biosciences (IAB)2 in Grenoble (southeastern France). As from the mid-20th century, “the biomedical model took over and focused more on treatments than on prevention”, she notes.
Pollutants in the dock
Nevertheless, pollutants were identified as factors for disease as from the 1940s, because – as Barouki says – “some teams were working on exposomic research without realising it”. Thus diethylstilbestrol (known as Distilbène in France), a synthetic oestrogen prescribed to prevent miscarriages in pregnant women until the 1970s, was shown to cause cancers of the reproductive organs and numerous other problems, including in the next generation. Research had already been carried out on the effects of exposure to asbestos, smoking and alcohol, before endocrine disruptors were also identified as a threat: “in the 1980s, biologists observed reproductive disorders in several animal species as well as impaired fertility in humans and longer periods required to conceive a first child”, explains Jean-Baptiste Fini, professor at the Molecular Physiology and Adaptation unit (PhyMA)3 of the French national museum of natural history.
Storage of molecules, continuous exposure and the cocktail effect
While epidemiological and toxicological research was initially limited to studying the effects of a single contaminant, exposomics now seeks to broaden this approach through a more holistic vision of exposure. With good reason: “We are now exposed to hundreds of molecules every day,” through three main vectors: air, water and diet. Some molecules are persistent: “they remain in the body, even if their levels fall in the blood,” stresses this specialist in endocrine disruptors, referring in particular to organochlorine products. Others, by contrast, are not stored, such as bisphenols or phthalates. “These substances are widely used but only remain in the body for around eight hours, unless we are exposed to them on a continuous basis.”
These disruptors interfere with hormonal messages sent to cells, either by preventing them from reaching their destination or by sending information at the wrong time. The effects of these products have been studied in humans, but “their consequences, notably following low exposure, are still poorly understood”, says Fini. Particularly since exposure to these disruptors can vary considerably depending on the period of life – childhood, adolescence, adulthood. And the task becomes even more complex when trying to understand the well-known “cocktail effect”, or the synergy that may occur in the body between different pollutants.
Delayed speech and effects on the thyroid hormone
To clarify the effects of a cocktail of endocrine disruptors on the brain, Fini and his team have studied a mixture of eight substances identified during a European project: five non-persistent disruptors such as phthalates (which are found in PVC) and three persistent ones such as perfluorinated compounds, used in stain removers, for example. “This mixture is found in the urine of women during pregnancy. In infants who are over-exposed in utero, a correlation has been made with signs of speech delay and a reduction in the number of words used at the age of 30 months,” the biologist explains. To verify this, the mixture was tested by their Italian colleagues on an in vitro model of the human brain. In this culture “we observed an overexpression of certain genes, already identified in cases of intellectual impairment”, he notes. To go further, this combination of substances was then tested on amphibians to clarify precisely which hormones it affected. To metamorphose into a frog, a tadpole is dependent on the thyroid hormone; when exposed to the eight contaminants, “its mobility was disturbed and it was no longer able to move correctly”, Fini adds, thus proving that these pollutants affected the said hormone. According to the scientist, characterising the synergy between molecules is a key point in the exposome: “If the regulatory evaluation of these products had been performed on the mixture, the acceptable doses of each chemical compound would have been lower than those currently used and 54% of pregnant women would not have been exposed to problematic quantities of this combination of endocrine disruptors.”

While the exposome promises to consider all exposures as a “whole”, toxicologists can already draw on new tools to take up this challenge; for example, mass spectrometry, which is a powerful and sensitive analytical technique that can detect minute traces of chemical compounds.
Analysing unknown substances
“Out of the 100,000 substances on sale in Europe, it is estimated that 500 are totally familiar, another 30,000 a bit less so, and that we know virtually nothing about the rest,” comments Barouki. “Mass spectrometry enables the analysis of several hundreds or even thousands of compounds at once,” including those whose presence was unsuspected. “This has led to a boom in the exposome approach,” insists Fini, because scientists are no longer limited to testing known molecules but also those that are unknown, in a sample of urine or blood, for example.
This tool also improves scientists’ understanding of the impact of xenobiotics – pesticides, medicines – on biological tissues, as it can screen for endogenous substances produced by the body following a contamination. In other words, it can detect the reaction of the organism to its exposome, such as an increase in inflammatory stress or the secretion of certain metabolites. In the longer term, elucidating how the exposome affects human health should make it possible to adapt regulations and health guidelines.
However, these changes require a considerable period of time, and although epidemiology can contribute to policy-making, “it is always playing catch-up because studies on exposures take several years,” warns Fini. “We have realised that the regulatory research carried out so far is incomplete because it was based on a substance-by-substance approach, which overlooked that fact that we are continually exposed to a mixture of molecules,” Barouki laments.

True enough, the complete mapping of a human exposome is laborious, notably because, unlike the genome and its 23 pairs of chromosomes, the exposome does not have a single substrate.
“Even if urine enables the assay of a thousand persistent substances, it will also be necessary to collect blood samples to determine more persistent compounds, to capture ionising radiation, and to deal with behaviour and psychosocial factors, etc., and all of this while taking account of the fact that these exposures change over time throughout a life. This is a much greater level of complexity than the genome,” insists the environmental epidemiologist Rémy Slama.
The director of the ITMO public health institute and co-director of the environmental epidemiology team at the IAB, he points out that “in terms of chemical substances, scientists are still a long way from obtaining a complete description of the exposome”.
Proven respiratory issues
Mathematical models are gradually being developed in order to try and anticipate the dynamics of contaminations in the course of a lifetime. “At the level of air quality, for example, such models are attempting to predict how humans will be affected in a particular region,” says Barouki. The relevance of monitoring the exposome of each individual over time is also justified by the explosion of chronic diseases seen in the context of the industrial and chemical revolution that combines pesticides, plastics and emissions of atmospheric pollutants. To characterise the impact of environmental factors on respiratory health, Siroux and her team have suggested studying the exposome by identifying exposure profiles: specific combinations of exposure factors based on statistical classification methods. The aim is to highlight groups of individuals whose profiles make them more likely to develop respiratory issues.
For example, based on data from the Nutrinet cohort which gathers more than 170,000 internet users, the team tried to establish the degree to which certain exposure profiles at very early stages of life – passive smoking, attendance at nursery, not growing up in a rural environment, large number of siblings (≥2) and breastfeeding – were associated with an increased risk of asthma in adulthood. Using the European Helix cohort – which follows 1200 mother-infant couples across Europe using biomarkers – Siroux’s research team had already assessed the influence of around a hundred pollutants on the respiratory tract of children aged 6 to 12 years. This analysis, which dates from 2019, suggested that prenatal exposure to perfluorinated compounds and postnatal exposure to several endocrine disruptors (ethylparaben and certain phthalate metabolites) affected respiratory function in childhood.
The curse of dimension
“However we are faced with measurement biases,” notes Siroux. “For example, in epidemiology, smoking status is easy to determine, unlike medium- or long-term exposure to certain chemical pollutants that disappear after a few hours.” In the context of exposomic research, “it is therefore difficult to truly rank the risk factors, and the effects of some of them on health may be largely underestimated in our studies because of measurement error”. Although the definition of the exposome has existed for more than fifteen years, the scientist feels that it is “still only a concept”. By trying to integrate this notion, epidemiological research encounters many methodological problems, starting with the management of data. “We need to collect more and more intelligence, but trying to advance on the exposome and increase the amount of information available should not have a detrimental effect on data quality”, she warns. “The incorrect measurement of exposures will make it impossible to quantify their true impact on health”.
Her colleague Slama also mentions the “curse of dimension”. To sum up, and paradoxically, the greater the number of factors to be taken into account in an exposome study, the less the ability to extract this information. Faced with the “pervasive exposome trend and the temptation to dilute research efforts by developing exposome approaches in a large number of projects”, Siroux advocates large-scale French cohorts of around 10,000 people or more. “These studies should be of high quality and involve the monitoring of biomarkers and precise assays in order to evaluate both environmental exposures and health parameters, and enable scientists from a variety of disciplines to interact.”
Antibiotic resistance and global health
Although the exposome approach aims to be holistic – integrating all environmental components that impact human health – it cannot overlook the health of the ecosystems within which the chemical and microbiological hazards are combined. In the Host-Pathogen Environnement Interactions laboratory (IHPE),4 Delphine Destoumieux-Garzon, a CNRS research professor, is seeking in particular to understand the role played by pollutants in the selection of genes for antibiotic resistance in marine environments. Working in Spain, Germany, and France as part of the European SPARE-SEA project, she is studying the pesticide and heavy metal contamination of oyster-breeding lagoons and estuaries. “For example, when these are situated close to wine-growing areas, large quantities of copper are found in the coastal waters around Europe. Copper is able to co-select genes for antibiotic resistance that will circulate in both wild and farmed animals, including oysters,” she explains.
Having sequenced the genomes of bacteria present in coastal environments and in the oysters farmed there, the research team has highlighted nearly 400 genes linked to antibiotic resistance. “We are now going to see how, under the effects of pollutants, this resistance could spread in the marine ecosystem and constitute an infectious risk to animal and human safety,” she adds. The exposome thus forms part of the concept of global health – or One Health – which combines human, animal and environmental wellbeing.
“Account must also be taken of the fact that our bodies contain microorganisms that are necessary to stay in good condition, notably via our microbiota. Modification of the latter following exposure to a pollutant can induce the onset of metabolic diseases in humans. The same applies to other animal species,” explains Destoumieux-Garzon. “Plants, animals and microorganisms within ecosystems are all exposed to the same contaminants. The notions of the exposome and One Health are indissociable.”
Environmental justice
In the future, account must be taken of the social, behavioural and psychological exposome, including all areas of research in the human and social sciences. “The issue of environmental justice is crucial,” confirms Slama. Because – and this is no surprise – the underprivileged accumulate risk factors, especially in “urban exposomes” that combine pollution, noise, heat and poverty.
A study in the UK has shown that on average, residents in the most disadvantaged areas were exposed to higher levels of nitrogen dioxide and fine particles. Other correlations have been established between low income and poor air quality in the home.
These inequalities are also observed during the first thousand days of life – a crucial period – when infants born in low-income families experience increased exposure to benzenes or nitrogen dioxide. “By contrast, green spaces have a highly positive impact that has been demonstrated from an epidemiological standpoint,” notes Barouki.
Despite major European research projects – and the inclusion in 2016 of the term exposome in French law – the concept is still in its early days. At present, characterising the complete exposome of an individual from conception to death seems unfeasible. To gather this huge amount of knowledge, scientists are now pleading for finance commensurate with this challenge. “Funding for the exposome is far lower than that which was allocated to the human genome sequencing project,” reminds Barouki, who is asking for true interdisciplinary programmes that can also integrate the impacts of “climate change, natural catastrophes, forest fires or biodiversity loss, which also constitute exposures for humans”.
Beyond the “all-genetic”
In the longer term, Siroux advocates changes to public health policies, “which at present do not insist enough on the cumulated effects of products or behaviours. For example, in terms of respiratory health, there are no real preventive methods. How can we prevent asthma? We don’t know”, insists this epidemiologist, who hopes that research on the exposome will give rise to messages designed to preserve population health.
Finally, for some philosophers such as Élodie Giroux, an epistemologist at the Faculty of Philosophy in Lyon (central eastern France) there is also a risk of an over-reductionist approach to the exposome. A desire to reduce it to what scientists are able to measure and quantify using their biotechnological tools – or just limit themselves to the internal chemical exposome to the detriment of the sources of exposure – is far from the initial holistic promise. “The holistic approach needs to be markedly qualified because many methodologies are adopted today under the reductionist logic of the human genome, almost seeking to sequence and molecularise the environment by focusing on the internal chemical exposome,” warns the researcher, who questions both the exhaustive ambitions of the exposome and the role being given to the social sciences. “Is the exposome a means to go beyond the biomedical model and the “all-genetic”? Or a way to integrate the environment in biomedical science and a molecular approach?” she questions.
- 1. “Complementing the Genome with an ‘Exposome’: The Outstanding Challenge of Environmental Exposure Measurement in Molecular Epidemiology”, Christopher Paul Wild, Cancer Epidemiol Biomarkers Prev (2005) 14 (8): 1847.
- 2. CNRS / INSERM / Université Grenoble Alpes.
- 3. CNRS /MNHN.
- 4. CNRS / Ifremer / Université de Perpignan via Domitia.
Explore more
Author
Léa Galanopoulo has a biology degree and is currently studying scientific journalism at Paris-Diderot university.