You are here
Muting tinnitus

Buzzing, hissing, creaking, ringing, clicking or humming; according to a recent French study, although 23 million French people over the age of 15 have experienced tinnitus once in their lives, between four and seven million of them suffer from it on a permanent basis. Among these, 30% endure severe or very severe discomfort that impacts their personal, family and social lives, as well as their professional activities. Indeed, another survey conducted by the JNA and France Acouphène associations and published in February 2024, showed that 16% of people had taken at least one day off work because of their tinnitus, and 11.4% had to change their job or working conditions.
Although tinnitus is an individual burden with often significant psychological consequences that may even lead to severe forms of depression, it also constitutes a social and economic plight. The total health insurance cost of each patient concerned can indeed reach an annual €296.75, with sufferers having to contribute an average €1079.85 per year. As an invisible disability that has long been neglected or even denied, tinnitus is now the subject of research designed to understand and characterise it, with a view to offering those affected improved management and better recognition.
A new definition of tinnitus
Better understanding the phenomenon means describing it more clearly, without trusting incomplete definitions. In the past, tinnitus tended to be characterised as auditory perceptions that occur without any sound stimulation in the environment (in other words, as phantom perceptions). Now, physicians and researchers, including Arnaud Norena, head of the neuronal and dynamic audition team at the Laboratory of Cognitive Neuroscience1, have proposed a new definition of the symptom2.
The long version of this definition is as follows: “Tinnitus is an auditory sensation without external sound stimulation or significance but which is identifiable from its sensory characteristics: localisation, intensity, frequency and timbre. It reflects a dysfunction of the auditory system and/or other structures that may interfere with it. Under the effects of cognitive or emotional processes, tinnitus can be an unpleasant experience that may impact quality of life. Its management may involve multidisciplinary skills.”
What this definition highlights first of all, and what makes it innovative, is that tinnitus cannot be fully characterised without taking account of its effects on the individual experiencing it at the sensory and cognitive or emotional levels. And this varies considerably from one person to another.
Professor Alain Londero, surgeon in the ear, nose and throat (ENT) and face and neck surgery department at Hôpital Européen Georges Pompidou in Paris, makes a distinction between having tinnitus and being disabled by it. “Tinnitus does not necessarily distress the person affected and the presence of intolerance – or not – raises some important questions. These notably concern the factors that make some people sensitive to tinnitus, and not others”.
“We all experience different sensations, such as mild or moderate pain or tinnitus, which constitute general ‘background noises’", comments Norena. “The question is how each person experiences the 'background noise' of tinnitus. This feeling, which is relatively weak in its subjective intensity, poses the question of why it can be such a devastating challenge for some subjects. Studying the clinical impact of tinnitus on an individual means entering a domain that no longer concerns just the neurosciences (which mainly focus on the neuronal messages triggered by this sensation) but also psychology or even philosophy.”
Objective and subjective tinnitus
To get back to the definition, which also reveals the diverse types of tinnitus and their causes: “There are two main types of tinnitus: objective and subjective,” explains Norena. “Indeed, there may be an acoustic source within the body: this is referred to as objective tinnitus, in particular when vessels near the cochlea generate a sound or vibrations that are captured by this cavity in the inner ear like any other sound. This form of tinnitus is relatively rare and only concerns between 5% and 10% of cases.” This so-called “pulsatile” tinnitus can be “cured using neurovascular treatments (embolisation, stents) or surgery”.
The second main type of tinnitus is “subjective”. “In this instance, there is no sound source”, explains Norena. “The sound sensation is underpinned by a neuronal signal. It is the auditory system that itself generates a ‘neural noise’, or in other words, spontaneous neuronal activity (not triggered by a sound) that causes this sensation.” More than half of the time, tinnitus is linked to hearing loss and hence a cochlear lesion3.
A large number of pathologies affecting different levels of the nervous system can lead to hearing loss and thus to subjective tinnitus4. At the level of the outer ear, this may be a blockage caused by earwax or a foreign body, etc.
In the middle ear, there may be perforation of the eardrum, serous otitis media (presence of an effusion without any symptoms of acute inflammation; editor’s note), cholesteatoma (tumour), otospongiosis (a disease of genetic origin that damages the bone tissue; editor’s note) and lesions of the auditory ossicles. Finally, the inner ear may be affected by ageing, trauma (mechanical, pressure, sound, emotional), fistula, labyrinthitis (inflammation), or ototoxic substances (which can cause deafness; editor’s note).
The auditory nerve can be impaired by tumours, vascular loops, neuropathy or Lyme’s disease. Finally, at a central level, cranial trauma, neurodegenerative disease or abnormal intracranial pressure may give rise to problems.
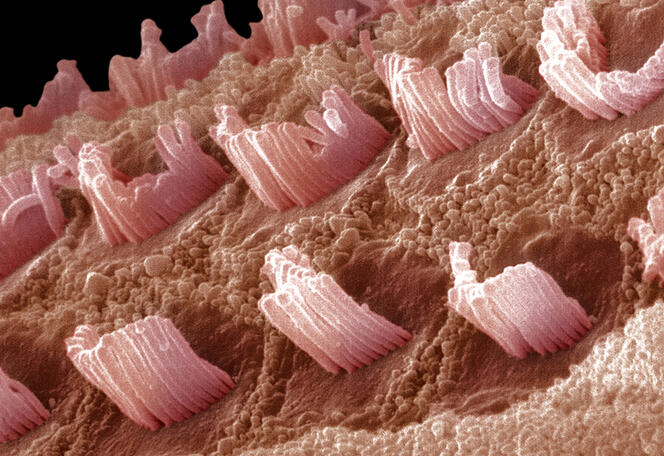
The brain responds to this loss of hearing by tinnitus, which is a sort of “aberrant” sensation, a little like an illusion. “The auditory system is ‘noisy’, at least at a peripheral level; in other words, there is a relatively high degree of spontaneous activity. This ‘noise’ is linked to the extreme sensitivity of the system,” Norena explains. “A cochlear lesion reduces it at a peripheral level, once the hair cells are affected. There is therefore less spontaneous activity in a silent state. This is paradoxical: although there is less noise, you can hear something!” In fact, in response to this reduction in sensory input, the brain seeks to adapt. This adaptation of sensitivity is achieved at the cost of an increase in spontaneous activity. “It is this surge in the auditory centres that gives rise to tinnitus, as a collateral effect of an adaptive process designed to maintain constant, normal neural activity. Tinnitus can therefore be considered as resulting from a compensatory mechanism,” he concludes. The symptom would therefore be a sort of bug in the brain caused by this organ’s attempts to adjust.
As well as the processes that govern the appearance of tinnitus, several factors may favour its onset (it is not necessarily permanent) and reinforce its perception, Londero details: “stress, sensations of fear or hypervigilance, fatigue, sleep disorders, exposure to noise, etc.”.
Primarily palliative treatments
And another cause was recently demonstrated: “Tinnitus can also be of somatosensory origin,” reveals Norena. “For example, when someone clenches their jaws or turns their head, tinnitus can intensify. The auditory system is then integrating sensory information that is not auditory but intero- or proprioceptive (for example, arising from the muscles). These non-auditory inputs, which may potentially increase because of the plasticity linked to hearing loss, may be ‘rerouted’ towards the auditory pathways and be interpreted as auditory sensations.”
This mechanism could in particular explain why some people who suffer from involuntary teeth grinding may also experience tinnitus. Although this somatosensory manifestations can be relieved by muscle relaxants, botulin toxin or even surgery, no specific treatment is available to relieve the symptoms of most of the individuals affected.
“At present, there is no therapeutic method – including medication – that can eradicate subjective tinnitus,” regrets Londero. “However, all sorts of palliative therapies can treat intolerance to tinnitus.”

“It is possible to use drugs intended to reduce anxiety, depression or sleep disorders, or that target causal pathologies such as Ménière’s disease,” the surgeon points out. “Sound therapies can also be proposed. These involve either compensating for hearing loss, or using sound enrichment techniques to mask the tinnitus. In this context, patients are often advised to go to sleep listening to a sound machine. It is also possible to use neuromodulation by magnetic and electrical stimulation5, but the results are inconsistent.” He explains: “The management methods derived from cognitive behavioural therapies (CBT) have received the best validation for enabling patients to better tolerate tinnitus.” It is in this context that a virtual reality immersion therapy has also been developed by his unit: “It allows a patient to interact with a sound that resembles their tinnitus, so that they can improve their tolerance of it.”
Towards drug therapies?
While Londero has much hope of improvements to auditory prostheses, Norena prefers to focus on potential drug treatments: “When studying the plasticity of the auditory system in animals, we became particularly interested in an inhibitory neurotransmitter called GABA (gamma-aminobutyric acid; editor’s note), and we realised that its inhibitory activity was modulated by another type of molecule called KCC2 (potassium chloride cotransporter 2; editor’s note). We were then able to show that KCC2 was down-regulated following hearing loss. This result is very interesting as it suggests that GABA, a neurotransmitter that is usually inhibitory, can become less inhibiting or even trigger excitation. These findings open pharmacological opportunities to restore the level of inhibition by increasing the activity of KCC2.”



Although current treatments for tinnitus are not entirely satisfactory, Londero encourages sufferers to consult a specialist, “firstly because the aetiology is sometimes curable, and secondly so that secondary prevention can be implemented to prevent tinnitus from becoming permanent and intensifying”. In conclusion, “Research on tinnitus is a relatively recent science when compared to the management of chronic pain, for example. What we need now is for it to become more structured.”♦
- 1. CNRS / Aix-Marseille Université.
- 2. https://doi.org/10.1016/bs.pbr.2021.01.029
- 3. A study in 2023 suggested that this percentage could be much higher because although no deficit was found on the audiogram, undetectable lesions may affect the auditory nerve fibres: https://doi.org/10.1038/s41598-023-46741-5
- 4. https://www.larevuedupraticien.fr/article/acouphenes-subjectifs
- 5. For example, headphones emit sounds that can reduce the perception of tinnitus, and at the same time, a system delivers small, painless electrical impulses to the tongue or jaw muscles.
















