You are here
What We Know about Pain

What is pain, what function does it serve and how can it be controlled? While this question is much more complex than it seems, biologists and neuroscientists are now trying to answer it, using the most recent exploratory technologies, such as MRI or magnetoencephalography to see how the brain functions, or electrophysiological studies to monitor the propagation of electrical signals in the nervous system, etc. “The limited advances achieved in analgesic treatments have led us to review our experimental approaches and explore the phenomenon in much greater depth,” observes Michel Barrot, a neuroscientist at the INCI.1
A sensory AND emotional experience
The definition of pain itself has been profoundly revised. According to the International Association for the Study of Pain (IASP), which brings together all physicians and scientists specialising in the field, pain is described as a “an unpleasant sensory AND emotional experience associated with actual or potential tissue damage”. Via the fibres that innervate the skin and organs, the body sends an electrical signal to the brain to warn it of a lesion (cut, burn, shock) that has occurred or is imminent — a veritable alarm system that preserves our bodily integrity. “People who are insensitive to pain — and this is actually a genetic pathology — live shorter lives: without pain, you can more easily injure or mutilate yourself,” points out Jean-Philippe Pin, a neuropharmacologist at the Institute for Functional Genomics (IGF).2
What is new in our approach to pain is the emotional component that was long underestimated by scientists. “When you cut your finger, there is no immediate pain. The electrical information travels to the brain and it is the cortex that interprets this signal as being painful," explains Michel Barrot. “In the absence of an unpleasant emotional experience, we refer to nociception rather than pain.”

Research in recent decades has shed light on pain circuits, or in other words, the neuronal mechanisms that capture and transmit the stimuli received by our skin and organs. About forty receptors and specialised pathways have been identified to date: some of them heat-sensitive (including those specifically reactive to temperatures higher than 47°C), some sensitive to cold or to mechanical pressure, etc., and others that are more generalist and keep watch over the “background” of the body. In real life, when you place your hand on a hotplate, several receptors and pathways are triggered at the same time: those active at more than 40°C, those that react at 47°C, those sensitive to the pressure exerted when you placed your hand on the hotplate, etc.,” explains Luis Garcia-Larrea, a neurophysiologist at the Hôpital Neurologique in Lyon, France.
The electrical signal generated by these receptors travels first of all to the spinal cord, where it is analysed. At this stage, the spinal cord may trigger a reflex action that causes withdrawal of the hand before there is any sensation of pain. This is the reflex arc. The second possibility is that the message is encoded by the spinal cord which transmits it to the brain to be interpreted. “Thanks to brain imaging, we now know that the message reaches both the regions of the brain that are specifically dedicated to sensory information, and those areas not specific to pain such as the attention region, the emotion regions responsible for unpleasant feelings, or the memory regions that seek to determine whether the individual has already been confronted with identical pain,” explains Luis Garcia-Larrea. “It is these latter areas that enable the stimulus to reach our consciousness and turn it into a real experience.”
A brain map of pain
The mapping of pain in the brain has now been achieved: "when you look at the brain regions that are active during a painful stimulus, you can see a ‘painful matrix’ that comprises around fifteen different zones of the brain, although we do not yet know the order in which these are activated”, suggests Luis Garcia-Larrea. In terms of emotions, two cortical areas are particularly important, the anterior cingulate cortex and the anterior insular cortex, as well as the subcortical amygdala. One thing is certain however, although the circuits followed by the painful signal are separate, the ultimate experience felt by the individual is definitely global.

Yet brain imaging cannot diagnose or quantify pain in a patient. "Pain is an eminently subjective experience, and perceptions of the same stimulus will differ from one individual to another, without us knowing whether this difference occurs at the level of the nociceptor circuits that transmit the sensory message or in the cerebral cortex itself,” explains Michel Barrot. The only way we have at present to evaluate pain is to ask a patient to mark it on a subjective scale (ranging generally from 0 to 10), a practice that is increasingly widespread in the clinic but has not always successfully reflected the suffering of patients.
Sensory information, however, does not just travel from the periphery to the brain. We now know that the brain itself is able to modulate how the spinal cord processes and encodes this information: this is the descending control of pain. “A good example of descending control is that of a wounded prey that runs to escape its predator,” explains Michel Barrot. “It does not feel the pain while fleeing, because the information has been “blocked” by the brain, whose sole priority is the animal’s survival. But it will feel it again as soon as there is no immediate danger.” The same prioritisation mechanism applies in the case of simultaneous pain; for example, if you have a bad back and you injure your hand with a kitchen knife, the second ache temporarily replaces the first.
This descending control generally takes the form of an electrical impulse (the most rapid) but can also travel via a hormonal pathway. INCI scientists have just shown that oxytocin — the attachment hormone that is also responsible for contractions during labour and the ejection of breast milk — can alleviate a painful sensation by acting on both the peripheral neurons that send the message to the brain, and on the spinal cord where the intensity of the signal is coded. The scientists have precisely identified thirty neurons located in the hypothalamus that coordinate the release of oxytocin into the blood and spinal cord. “Unfortunately, oxytocin cannot be used therapeutically, because it plays numerous other roles in the body,” points out Michel Barrot. “We nevertheless know that physicians who have administered it via the epidural route succeeded in reducing a patient’s pain.”



Although scientists are increasingly familiar with the circuits for acute pain, the same is not true of chronic or pathological pain that is not caused by a tissue lesion or that persists long after such strain has disappeared. These are neuropathies linked to a lesion of the nervous system itself; examples include the phantom pain that haunts nearly 15% of people who have undergone the amputation of a limb, diabetic neuropathy, discomfort caused by irritable bowel syndrome, or fibromyalgia, the generalised musculoskeletal pain syndrome that mainly affects women.
The challenges of chronic pain
Difficult to grasp, the mechanisms underlying chronic pain are now a focus for research scientists. “Chronic and acute pain share the same pathways, but there is a greater emotional component in the former,” suggests Luis Garcia-Larrea. Its true role continues to elude scientists: what is its purpose, knowing that it is not a matter in this case of protecting the body from imminent danger? As for its management, it also remains unsatisfactory.
“Some antidepressants, as well as drugs for epilepsy, have been used since the 1960s, and are able to relieve between 30% and 50% of patients suffering from neuropathic pain,” notes Michel Barrot. A mystery for many years, their action is now better understood, thanks notably to work carried out in his laboratory. “Although they are classified as antidepressants, these molecules — such as duloxetine or amitriptyline — do not just act on the central nervous system,” he explains. “They also influence the descending control of pain and the mechanisms underpinning the neurological inflammation that accompanies nerve lesions.”

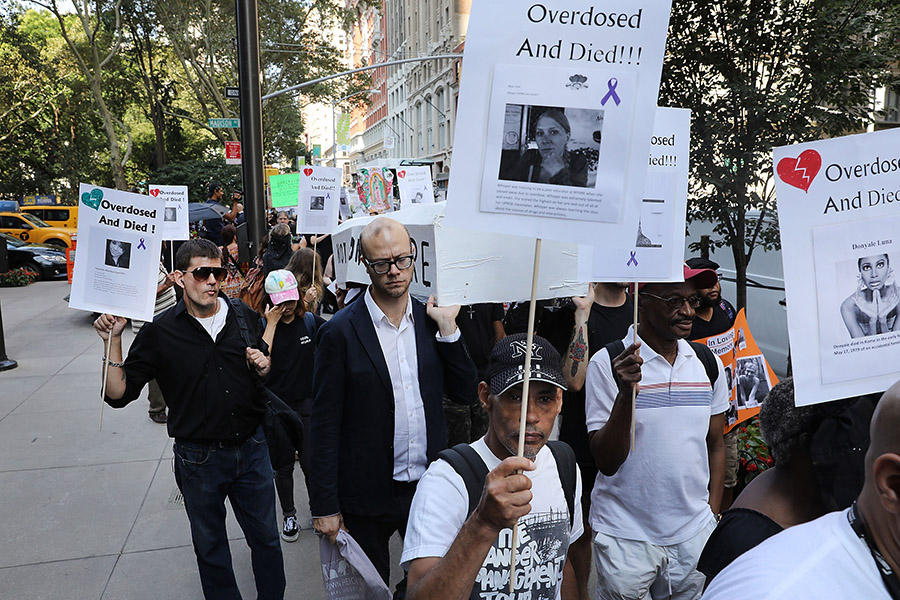
Since the end of the 2000s, opioid drugs previously reserved for very severe acute pain and palliative care have increasingly been prescribed to manage chronic pain. But they are not without danger: the efficacy of molecules such as morphine, codeine or tramadol, etc. decreases over time (hence the temptation to increase the doses), resulting in severe habituation and adverse effects such as nausea, constipation and respiratory distress which may have a fatal outcome. In the US, where these drugs are widely prescribed, they are thought to have caused 74,000 deaths from overdose during 2017 alone.
Are there alternatives to opioids?
One of the options being considered in response to this crisis may be the use of “biased” opioids. A molecule that mimics morphine, without its negative effects, is under study in the US. “Morphine is like a key that activates two different pathways in a cell, the anti-pain pathway A, and the B pathway responsible for addiction and respiratory effects,” explains Jean-Philippe Pin. “The idea is to create a molecule that resembles morphine but lacks that part of the key which activates the effects of habituation.”
Nanodrugs may also offer an alternative to morphine, as has just been shown by a team of French scientists at the Institut Galien Paris-Sud.3 By binding a peptide (leu-enkephalin, which is usually broken down within a few minutes in the body) with a natural lipid (squalene), these researchers have succeeded in creating nanoparticles that are active for up to 48 hours; they are able to target the opioid receptors and eliminate pain related to prolonged inflammation in rats. The advantage of this treatment — should its efficacy be proved in humans — is that "unlike morphine, these nanoparticles are too large to cross the blood-brain barrier and therefore do not penetrate into the central nervous system,” explains Patrick Couvreur, who co-signed the study. “In this way, addiction and respiratory distress can be avoided.”
“In the case of neuropathic pain, such as diabetic neuropathy, nerve traumas or phantom limb pain, local anaesthetics such as lidocaine can also be used, applied in a cream to the painful area,” adds Luis Garcia-Larrea. Preparations based on capsaicin, the active molecule in chilli peppers, have also demonstrated some efficacy. “The painful legs experienced by paraplegic or amputated patients is actually due to the fact that the nervous system tries and fails to regenerate the sectioned fibres, leading to over-excitation of the entire system,” the physician explains. “And scientists have discovered that TRVP1, a peripheral receptor sensitive to heat, responds well to capsaicin at very high concentrations.” The aim is to over-excite these receptors to the point that they are inactivated, and thus offer a few weeks’ respite to a patient who is suffering.
At the IGF, Cyril Goudet is focusing his research on the amygdala, the brain structure that plays an important role in responses to aches and stress. In mice suffering from neuropathic pain (in this case, long-term inflammation of the paws) he has shown that it is possible to eliminate discomfort by acting on the glutamate-sensitive receptors located in the amygdala. “The problem with using models such as the rat or mouse is that it is impossible to reproduce the same protocols in humans in order to verify our hypotheses. Treatments that were effective in mice have already proved useless in humans," explains Jean-Philippe Pin, who also uses these rodents to explore the opportunities offered by light-controlled drugs: molecules delivered to the centre of the brain that could be WIFI-activated via micro-LEDs implanted in the cortex, etc.

Faced with the current limitations of pharmacology, other options are also being developed to alleviate suffering from chronic pain. These include neuromodulation, which consists in modifying electrical activity at precise points in the nervous system — either in the spinal cord or directly in the cerebral cortex — and which can provide relief to about half of patients experiencing this pain. “We now know that there is not just one but several pain centres in the brain,” explains Luis Garcia-Larrea. “The aim is to alter electrical activity in the three or four cortical regions responsible for unpleasant sensations.” This can either be by implanting electrodes — transcranial direct current stimulation, or tDCS — or using an electromagnetic coil that stimulates the interior of the brain — repetitive transcranial magnetic stimulation, or rTMS. “Although it is less invasive than stimulation using electrodes, the latter is less powerful as it is more distant from the centres targeted,” the scientist points out.
Hypnosis and meditation
Other less orthodox methods are also being investigated as they have a direct effect on the experience of pain, such as hypnosis and meditation, which are now being taken very seriously by scientists. “The idea is not to eliminate the cause but the feeling, by acting on two particularly important regions of the cortex, the anterior cingulate cortex and insular cortex, which are activated during a painful experience,” explains Rémy Schlichter, Professor of Neurosciences at the Université de Strasbourg (northeastern France). “Indeed, these regions help the central nervous system to decide whether a stimulus is important or not.” The aim of these techniques is therefore to confuse the system and thus prevent any potentially painful information from reaching our consciousness.
“The brain can only process a limited number of pieces of information in parallel; about six or seven,” details Rémy Schlichter. “By focusing attention on breathing, or a particular part of the body, meditating when conscious alters the cognitive state of the brain, which — busy processing this piece of information — is unable to deal with others.” Hypnosis follows a similar logic, the aim being to dissociate sensory aspects (nociceptive circuits) from emotional experience, and to reassociate another context with the stimulus, in order to change its interpretation.
“Until recently, hypnosis was considered as charlatanism by many doctors,” the researcher goes on, “but it was saved by advances in medical imaging.” Increasingly employed in the management of chronic pain, hypnosis is also used in the operating room where in some situations, and in patients who are particularly receptive to hypnotic suggestion, it can replace general anaesthesia. This was notably the case of a surgical procedure on the thyroid that was carried out at Hôpital Henri Mondor in Créteil (near Paris) under hypnosis and local anaesthesia: the patient, a professional singer, was able to sing during the procedure and thus prevent her vocal cords from being affected by the surgery. Even so, the physiological mechanisms underlying hypnosis still need to be clarified. “In most cases, the regions of the brain that are seen to be activated or inactivated during a session of hypnosis are not specific to this condition, which complicates the study of the phenomenon,” explains Rémy Schlichter.
Despite the numerous options being investigated, pain is far from having revealed all its secrets.