You are here
How light governs sleep
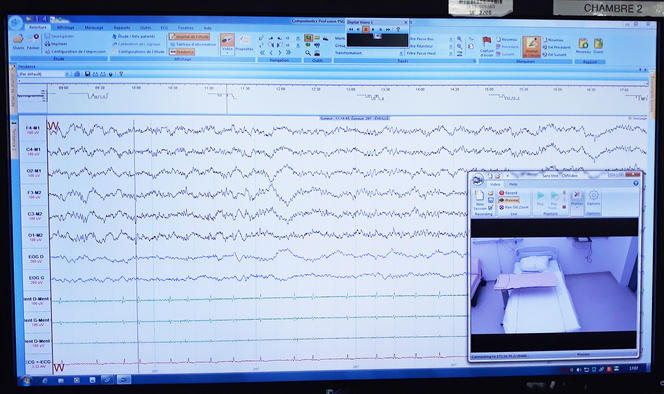
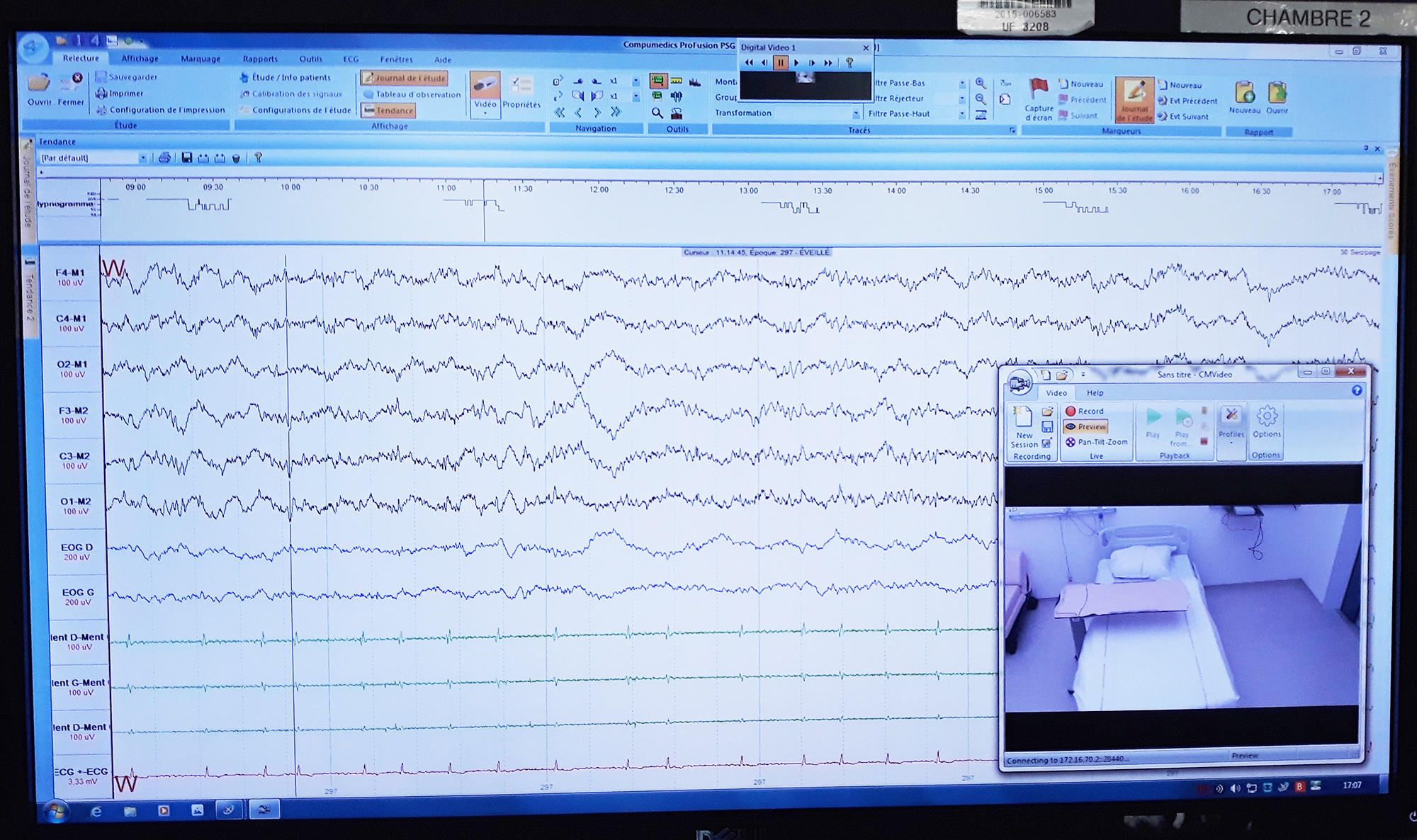
With its ten screens, one per room and per patient, the nurses’ station at the CIRCSom looks like a high-tech control tower. Day and night, the staff monitors the patients’ recordings and ensures that their stay in the hospital goes smoothly. It usually takes two nights and two days to make a diagnosis and propose a course of treatment. “It’s a little different for the healthy volunteers admitted as part of a research protocol, who might stay as long as a week,” says Laurence Hugueny, the centre’s coordinator and our guide for an insider’s tour of this unique facility – both a sleep clinic and a research centre. The CIRCSom admits patients suffering from circadian rhythm disorders, disruptions of the system that controls the sleep-wake cycle, as well as volunteers with no sleep pathologies. The researchers’ goal is to gain a better understanding of how sleep works, in order to improve it.
Tools to map the night
Sleep is a mystery to the outside observer, for whom it is nearly impossible to tell which phase a sleeping person is experiencing – light sleep, slow-wave sleep or REM sleep – and whether this approximately 90-minute cycle is repeated uninterrupted until the dreaded ring of the alarm clock. Fortunately for doctors and researchers, a number of physiological parameters provide precious indications: the brain waves are slowest during slow-wave sleep, while muscle tone is lowest during the REM (also called “paradoxical”) phase, etc.
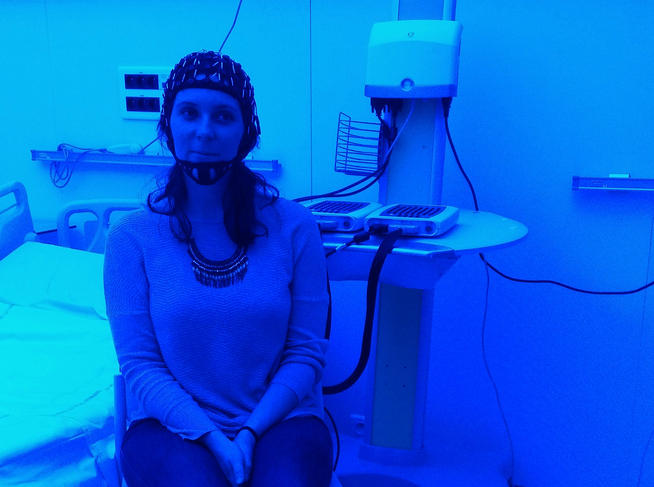
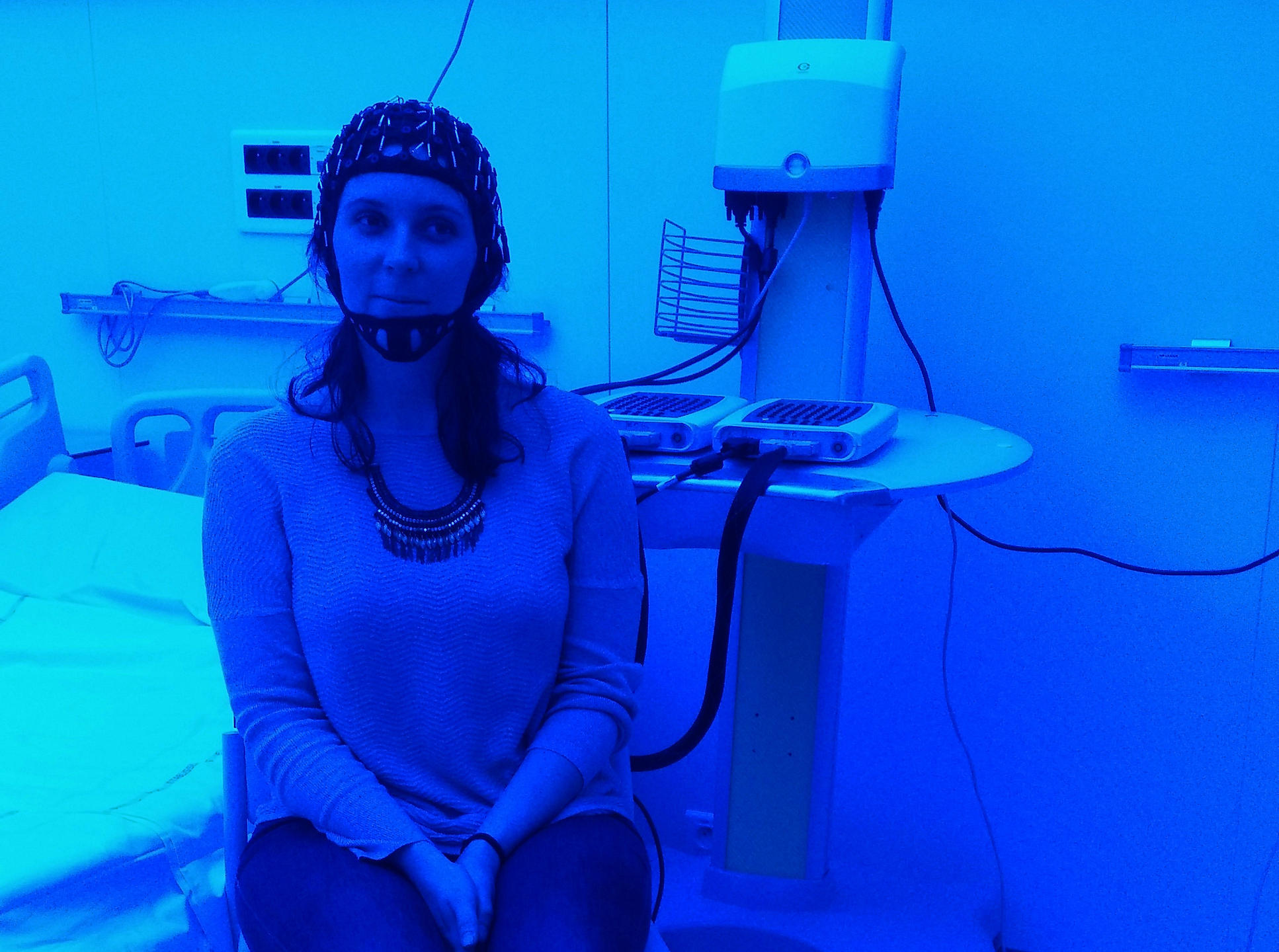
Patients and research volunteers alike have to accept being fitted out from head to toe during their stay at the CIRCSom. The ideal tool for unravelling the secrets of our sleep is polysomnography, a system that combines an electroencephalogram (EEG) to record the brain’s electrical activity, an electrooculogram (EOG) to detect the movements of the eyeballs, and an electromyogram (EMG) attached to the chin to monitor its muscular activity during sleep. In other words, a lot of wires and electrodes to hook up! To which could be added, depending on the indications, an electrocardiogram to measure the subject’s cardiac activity, two additional electromyograms on the legs to monitor their movements, and of course cannulas attached under the nose to assess respiratory flow.
Indispensable for both clinical treatments and research, polysomnography provides an accurate record of the night’s sleep. But the CIRCSom’s unique field of expertise, the activity that makes it the only research centre of its kind in France, is the study of light: how it is involved in the regulation of sleep and how it can help in the treatment of certain sleep disorders through luminotherapy. “Twenty years ago it was thought that the 24-hour sleep-wake cycle was regulated solely by our biological clock,” recounts CIRCSom director Patrice Bourgin. “We only knew about the visual functions of light. Today this belief has been disproved. We know that light – its colour, its intensity, the amount of time we are exposed to it – directly influences our sleep, even though research on the subject is still in its infancy. A lot remains to be discovered…”
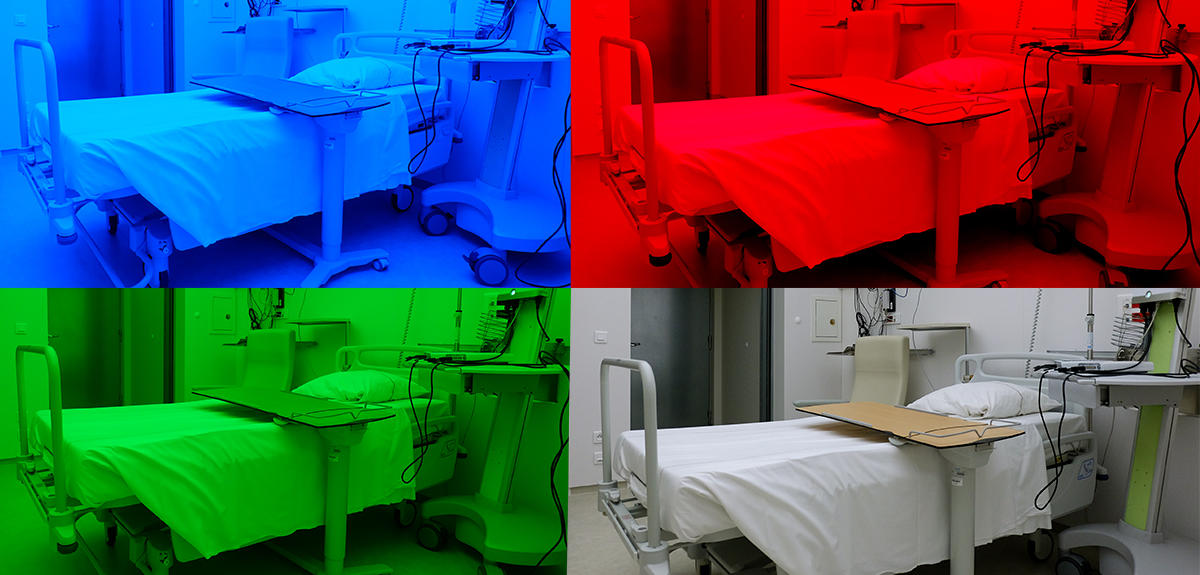
Hospital rooms with modulable lighting
The researchers needed a tool to study the effects of light on the quality of sleep. The CIRCSom has ten hospital rooms, five of which are “chronobiology rooms”, we are told as we pass through a double door to enter a windowless chamber. Inside, the luminosity is determined not by the sun but by the scientists themselves. “With the LEDs mounted in the ceiling, we can ensure perfectly uniform illumination and modulate the lighting of the room as we like – from red to green to blue, or polychromatic white comparable to daylight,” Bourgin explains, while the demonstration programme suddenly immerses us in a bright red glow. Opened in 2016, these cosy cocoons, insulated from the outside world by ultra-effective soundproofing (-70 decibels), are the fruit of nearly seven years of development in collaboration with a private partner. “Hidden in a two-metre space above the false ceiling is all the cooling equipment – even the LEDs produce heat – plus humidity sensors and the IT installation,” the research physician tells us. “The data flow that we generate is enormous, equivalent to that of the entire hospital.”
To the left of the double-door entrance hall, which is lit with the same colour as the room itself (including its bathroom and toilet), a small hatch in the wall makes it possible to take blood samples at any time of the day or night without waking the patient, who is fitted with an arm catheter. This system allows the researchers to measure the two key hormones involved in the sleep-wake cycle: melatonin, the hormone of darkness, which helps us fall and stay asleep, and cortisol, which promotes wakefulness and reaches peak production at about 8:00 am.
Three factors regulate the sleep-wake cycle. The first is the 24-hour circadian rhythm driven by our internal biological clock. “It’s nearly like fingerprints, specific to each individual,” Bourgin says. “Some people are evening chronotypes, who go to sleep late and get up late, while others are morning chronotypes, waking up early and going to bed early. Some are short sleepers who need less than eight hours of sleep a night, which is the average time needed for an adult, and others are long sleepers.” The second factor to be considered is “homeostatic pressure”: the longer we stay awake, the greater the sleep-wake imbalance, and the more we feel the need to sleep.
The third and last factor involved in the sleep-wake cycle is the external synchronisers linked to our environment: social interactions, physical activity, noise, food intake and – most importantly – light, the focus of the CIRCSom’s research. The light we are exposed to helps our biological clock adjust, for example after a transatlantic flight. In a study conducted on rodents, published in June 2021, the centre’s team went further, showing that the direct effect of light accounts for more than half of the sleep regulation mechanism – much more than they had expected! To ensure a good night’s sleep, it is thus essential to get enough exposure to daylight. And not just the daylight that comes through the windows of an office or a house, whose quantity does not exceed a few hundred lux during the day, but rather overhead daylight, in other words outdoors, where even in cloudy conditions the luminous flux reaches 1,000 to 2,000 lux – and as much as 100,000 lux on a sunny summer day.
“One of our main areas of research at the CIRCSom consists in investigating the effects of the various wavelengths of the light spectrum – blue, red, green… in the long-term”, Bourgin says. “The goal is to identify how each one influences our rhythms depending on the time of day we are exposed to them, as well as our degree of sleep deprivation.” With one-third of today’s salaried employees working shifts, in addition to the jet lag linked to intercontinental air travel, the widespread use of artificial light, light from screens, etc., more and more people suffer from pathologies related to circadian rhythm disorders. As an example, the physician cites a recent case: “I was consulted by a lorry driver whose circadian rhythm was so completely disrupted that he could no longer sleep at night.”

Rhythms and blue
Raphaëlle Glacet, a PhD student at the CIRCSom, specialising in the neurosciences, has decided to devote her doctoral thesis to the effects of blue-enriched white light. Contrary to the common belief that red is stimulating, while blue is a soothing colour used for example in night lights for children’s bedrooms, the opposite is actually true. “We know that blue-enriched white is an ‘active’ light to which a specific photopigment in our retinas, melanopsin, is especially sensitive,” the researcher says. “My study aims to determine how this wavelength influences our cerebral activity, cognitive performance and sleep-wake cycles, depending on the circadian time and our level of sleep deprivation.”
In order to more accurately assess the influence of blue light, Glacet asked volunteers to spend 40 uninterrupted hours in the hospital’s chronobiology rooms. One of the groups was deprived of sleep for all 40 hours, while the other alternated naps with waking periods. Within each group, half of the volunteers were exposed to a “neutral” muted light with no physiological effect, and the other half to blue-enriched white light. During the test, they were asked at regular intervals to perform short exercises in alertness and problem solving.
“One of the things we wanted to find out was to what extent the blue-enriched light reduced somnolence during a night of sleep deprivation and at what point it ceased to be effective,” Glacet explains, “especially during the crucial hours around 5:00 am, when the circadian rhythm and homeostatic pressure inexorably prompt us to sleep.” The scientist also investigated whether exposure to blue light as a means of stimulating alertness in the middle of the night (which could be of use, for example, to night workers) hinders resting a few hours later. “On this second point, the initial results tend to indicate that this is not the case, but it has yet to be confirmed,” says the researcher, who plans to publish her thesis this winter.
Similar studies on other wavelengths are set to follow soon. Discerning the role of each one in disruptions of the 24-hour sleep-wake cycle – the core area of expertise of the physicians at the CIRCSom – should make it possible to expand the applications of luminotherapy, whose benefits are already well established for certain disorders like advanced and delayed sleep phase syndromes.
Luminotherapy and phase disorders
“Delayed sleep phase syndrome affects 3 to 5% of the population,” explains the CIRCSom somnologist Ulker Huck, “and is mainly observed among teenagers, who have a natural tendency to go to sleep late at night and wake up late in the morning. If they are already evening chronotypes by nature, their sleep cycles can become totally disrupted, to the point of their not being able to get up and go to school in the morning. Advanced sleep phase syndrome, on the other hand, impacts about 1% of the population, mostly older people who were already morning chronotypes, and will get very sleepy as early as 8:00 pm but will wake up at 3:00 am!”
In both cases, the disruption can be treated by the right kind of luminotherapy. For delayed phase syndrome sufferers, this means exposure to high-intensity light (10,000 lux) from a luminotherapy lamp for 30 minutes after waking up, wearing sunglasses in the evening and avoiding screens for two hours before bedtime. Conversely, those with advanced phase syndrome are advised to wear sunglasses in the morning, in order to minimise the quantity of light received, expose themselves to light in the evening and, if desired, take a nap in the afternoon to reduce homeostatic pressure.
Luminotherapy could have many other indications as well, in particular for certain comorbidities linked to sleep disorders. “We are studying its effects on the non-motor symptoms of Parkinson’s disease, autism and depression,” Bourgin reports. “Concerning the latter, a recent analysis of all the studies conducted on the subject shows that luminotherapy is as effective as antidepressants.” On the other hand, the question of its use in patients suffering from insomnia is still under study. “Very little work has been done on the subject, with too small cohorts,” the researcher says. “We have several research protocols underway, involving more than 350 patients in three different parts of the country, to see how luminotherapy administered in the morning can alleviate insomnia. The effects of the different wavelengths are also being examined.”
This is a mammoth –yet much needed – task in our modern-day societies. “Nowadays, sleep is sacrificed,” Hugueny comments, pointing out that the average French adult gets fewer than seven hours of sleep per night. “It’s a real challenge for the future, especially because our constantly increasing exposure to artificial light and the ever-wider use of colour LEDs is liable to make things worse.”
__________________________________________________________
Sleep disorders in children
Patients in the CIRCSom waiting room often include very young children. In their case, “disruptions of the circadian rhythm are frequently linked to the presence of neurodevelopmental problems”, explains Huck. One difficulty that must not be underestimated is that sleep is essential for emotional development and learning, as well as for growth. Production of the growth hormone reaches a peak during the slow-wave sleep phase. “Some children diagnosed as having ‘attention deficit hyperactivity disorder’ actually suffer from sleep problems that need to be treated,” the scientist adds. Children with autism also experience difficulties in falling and staying asleep. “These problems are relatively common and must be addressed,” she concludes. “Treating them can have a favourable effect on behavioural disorders during the day.”